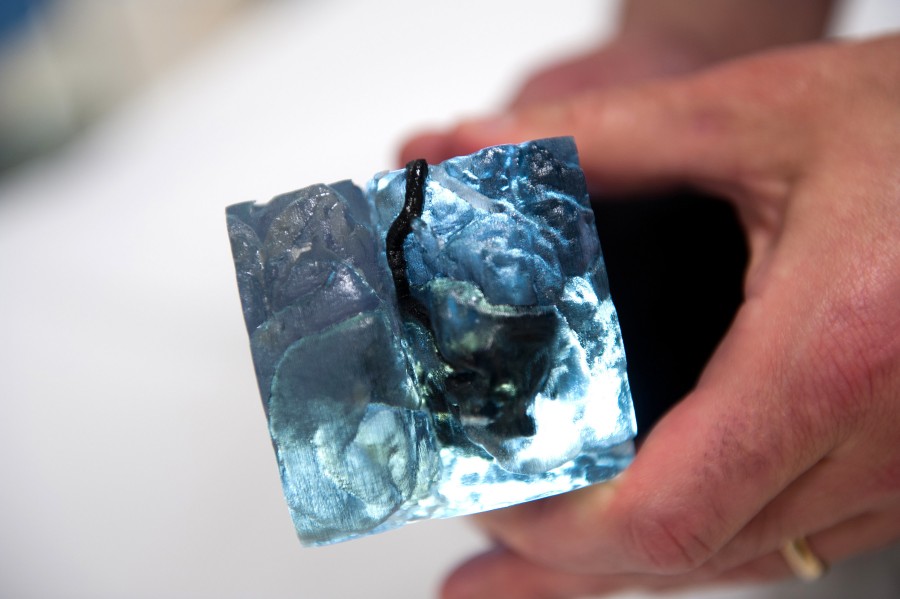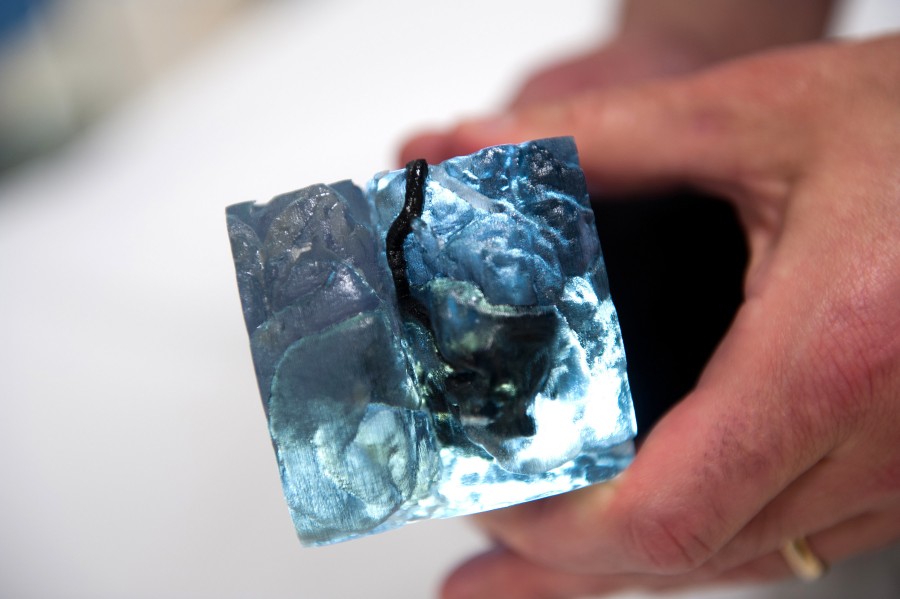
A 3D-printed arteriovenous malformation (AVM) shown embedded in the surrounding brain tissue
Credit: Boston Children’s Hospital
3D Printing is not just for the tech world; it’s changing lives in medicine.
Boston Children’s Hospital physicians report the first cases of children benefiting from 3D printing of their anatomy before undergoing high-risk brain procedures. The four children had life-threatening cerebrovascular malformations (abnormalities in the brain’s blood vessels) that posed special treatment challenges.
Reporting online today in the Journal of Neurosurgery: Pediatrics, the physicians describe the use of 3D printing and synthetic resins to create custom, high-fidelity models of the children’s vessel malformations along with nearby normal blood vessels. In some cases, the surrounding brain anatomy was also printed.
“These children had unique anatomy with deep vessels that were very tricky to operate on,” says Boston Children’s neurosurgeon Edward Smith, MD, senior author of the paper and co-director of the hospital’s Cerebrovascular Surgery and Interventions Center. “The 3D-printed models allowed us to rehearse the cases beforehand and reduce operative risk as much as we could.”
The children ranged in age from 2 months to 16 years old. Three of the four children had arteriovenous malformations (AVMs), in which tangles of arteries and veins connect abnormally, and were treated surgically.
“AVMs are high-risk cases and it’s helpful to know the anatomy so we can cut the vessels in the right sequence, as quickly and efficiently as possible,” says Smith. “You can physically hold the 3D models, view them from different angles, practice the operation with real instruments and get tactile feedback.”
The 2-month-old infant had a rare vein of Galen malformation in which arteries connect directly with veins—bypassing the capillaries—and was treated with an interventional radiology technique to seal off the malformed blood vessels from the inside.
“Even for a radiologist who is comfortable working with and extrapolating from images on the computer to the patient, turning over a 3D model in your hand is transformative,” says Darren Orbach, MD, PhD, chief of Interventional and Neurointerventional Radiology at Boston Children’s and co-director of the Cerebrovascular Surgery and Interventions Center. “Our brains work in three dimensions, and treatment planning with a printed model takes on an intuitive feel that it cannot otherwise have.”
The life-sized and enlarged 3D models were created in collaboration with the Boston Children’s Hospital Simulator Program (SIMPeds) using brain magnetic resonance (MR) and MR arteriography data from each child. Measurements of the models showed 98 percent agreement with the children’s actual anatomy.
All four children’s malformations were successfully removed or eliminated with no complications.